At the Medanets User Days in February, Solution Expert Suvi Airaksinen from the wellbeing services county of Central Finland shared some of the best practices for deploying new pharmacotherapy policies and the Medanets Medication mobile solution. We also put together tips from our other customers in this article.
The requirements set for documenting medication administration are already quite high, and they will only get stricter in the future. This is because errors in medication management are one of the major reasons for adverse events and patient injuries around the world1. In practice, it can be challenging to ensure that entries are made in accordance with all the requirements.
Mobile solutions supplementing EHR systems can help achieve the goals of safe pharmacotherapy and enable up-to-date, structured medication administration entries in line with the strictest requirements. In the future, they can also act as part of the closed loop medication process.
Even though the Medanets Medication solution is easy to use in terms of technology, its deployment often entails process changes, the implementation of which calls for thorough consideration. Here are some tips from our customers:
- Be clear about the goal and explain the reasons for the changes.
- Define the policy at a sufficiently high organisational level.
- In training, tap into the expertise of clinical experts and change agents.
- Ensure internal information flow.
- Offer sufficiently detailed instructions to users.
- Ensure know-how in theory and practice.
- Be patient about expanding usage.
1. Be clear about the goal and explain the reasons for the changes
The deployment of the Medication solution usually means adding another step to the nurses’ workflow. That is why it is important to unambiguously explain to everyone why the new step is important and what the goal is.
An assessment of the current state and the desired future state can be used to support the start of the process. Find an example of an assessment template below. We can also send a template you can fill in to your organisation, if desired.
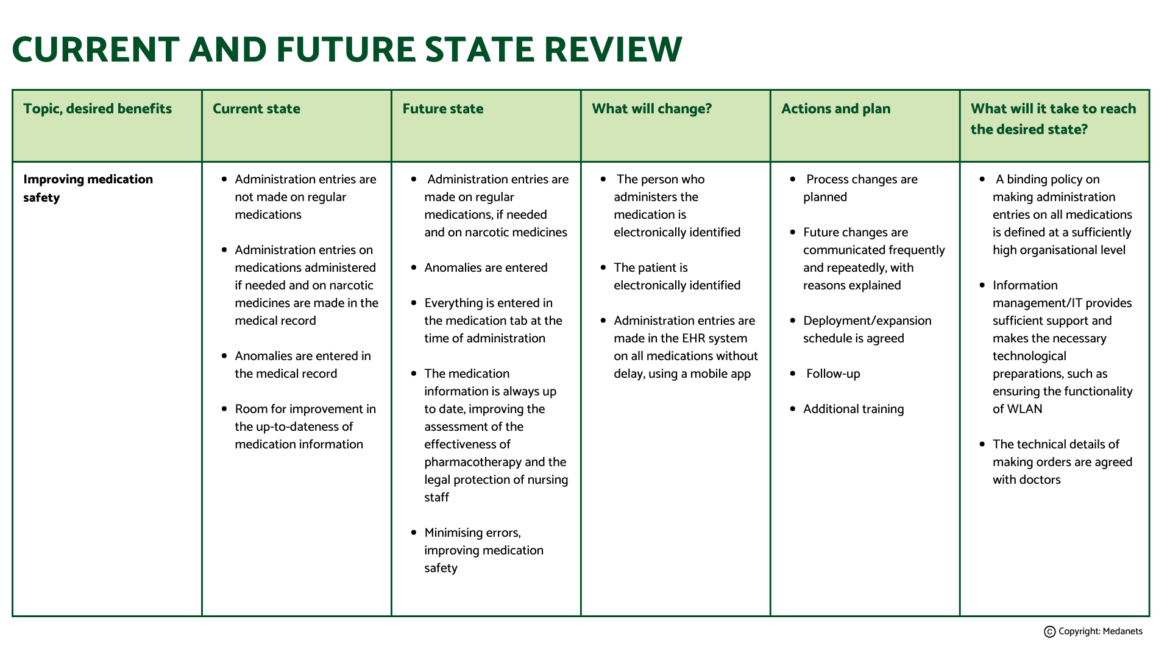
Click on image to enlarge
As the deployment process proceeds, remember to reassess the current and desired status every once in a while; where are we right now in terms of reaching our goals? What else needs to be done before we reach the desired results?
2. Define the policy at a sufficiently high organisational level
Many of our customers have noticed that reaching the goal requires a policy defined at a sufficiently high organisational level. For example, to improve patient safety, the organisation can decide that administration entries must be made on all medications. In Central Finland, for example, this type of a policy is included in a guideline common to the whole region: administration entries are made on all medications in the units that use the Medanets Medication. With this policy, the wellbeing services county aims to increase medication safety, develop the pharmacotherapy policies towards the closed loop medication process and to speed up the documentation of administration entries.
If desired, the nursing staff can be offered freedom in the implementation the policy, as long as the organisation ensures appropriate compliance. For example, the staff can be offered various tools for the practical implementation of the policy, such as making administration entries using a workstation or a mobile device. The method that proves to be the most useful in practice will become the norm.
3. In training, tap into the expertise of clinical experts and change agents
In addition to technical specialists, Medanets also provides clinical experts to support deployment and training. Our customers have found them extremely helpful, particularly in more challenging deployments.
It is also a good idea to build a network of internal change agents3within the organisation, and use them both for training and for the overall change process. Many of our customers have benefited from naming responsible persons for Medanets. Ideally, each ward has its own responsible person, ’Medanets champion’. The Medanets champion is someone who has received extensive training in the use of the Medanets application. This person will be the direct support of the ward nurses in situations related to the application, thus lowering the threshold for requesting help. Being a Medanets champion has been seen as a much-needed boost to the regular work, giving the employee an opportunity to develop their skills.
4. Ensure internal information flow
It is vitally important to communicate any changes. In all communications, remember to explain the reasons and repeat the core message as many times as is needed.
In Central Finland, on of the changes was the decision to record the medication administration in only one place in the EHR system. This change was linked to the change of version of the EHR and was accompanied by extensive training sessions, which also supported the information flow.
It is crucially important to ensure that all the professional groups are up to date and aware of how the changes will affect them and what roles they play in implementing the changes. The nurse makes the administration entries, but in order for the prescribed medications to have the right format in the medication record so that the administration entries can be made, the doctors must also be encouraged to support the change and instructed on the correct procedure for issuing prescriptions. It is also a good idea to unambiguously agree on the division of labour between nurses and doctors; who makes the necessary changes in the system if an order has been accidentally made in the wrong format?
Support functions, such as information management, must also be informed of changes at an early stage so that they can create the technological prerequisites for making the changes.
5. Offer sufficiently detailed instructions to users
Our customers have noticed that providing very detailed instructions on specific technical details makes the administration entries more efficient.
In particular, we recommend specifying the parts of the EHR system the information must be entered in and the correct format for making the entry so that the entries are displayed correctly and as desired anywhere where they need to be accessed, such as the Medanets app. These may include:
- entries in the comments section of the medication record
- dose entries and dose units of specific medications (for example, whether to record the dose in milligrams or tablets).
In Medanets, the administration entry must always contain numeric information on the administered dose. The instructions on how to record the information may vary. In addition, the entries of specific types of medications may have their own special characteristics that require separate instructions. These may include:
- transdermal patches and other medications not administered on a daily basis
- PCA pumps
- opioid medications
- intravenous antibiotics
- thrombosis prophylaxis.
Furthermore, it is a good idea to define a policy for how to record medications not included in the medication record and to provide instructions on deleting or editing an administration entry.
6. Ensure know-how in theory and practice
From the point of view of patient safety and efficient practical work, it is important to ensure that healthcare professionals have sufficient theoretical and practical competence concerning pharmacotherapy2 and the digital solutions used in pharmacotherapy. The Medanets app is a medical device, and there are specific rules for ensuring competence concerning medical devices. Tools have been developed for ensuring competence; one of them is called the device passport. In Kanta-Häme, device passports are used to ensure employees’ competence in using various types of medical devices.
7. Be patient about expanding the usage
If possible, stagger the deployment from unit to unit or from ward to ward. in Central Finland, it was discovered that a deliberate pace in the deployment allows close side-by-side teaching and training and ensures that everyone understands the new policy. Of course, the deployment can also be carried out faster or everywhere all at once; however, in that case, the user base must have good overall skills and the units must be able to offer sufficient support.
References:
1. Elliott et al. (2021): Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Quality of Safety 30: 96–105.
2. Finnish Centre for Client and Patient Safety: Osaamisen varmistamisen periaatteet. Cited 15 March 2024.
